Abstract
Background: Post-transplant lymphoproliferative disorders (PTLD) are a heterogenous group of various lymphoproliferative disorders arising after organ transplant. With the advances seen in transplant medicine, the use of solid organ transplant (SOT) and allotransplant have risen in the past decade and thus the incidence of PTLD. Prior studies have shown that patients with SOT are at 2-5-fold higher risk of developing a cancer than general population. PTLD is the most common malignancy after skin cancer in SOT patients and the most common cause of cancer related mortality amongst them. Herein, we describe the incidence, treatment pathways, and survival outcomes of PTLD arising from various SOT.
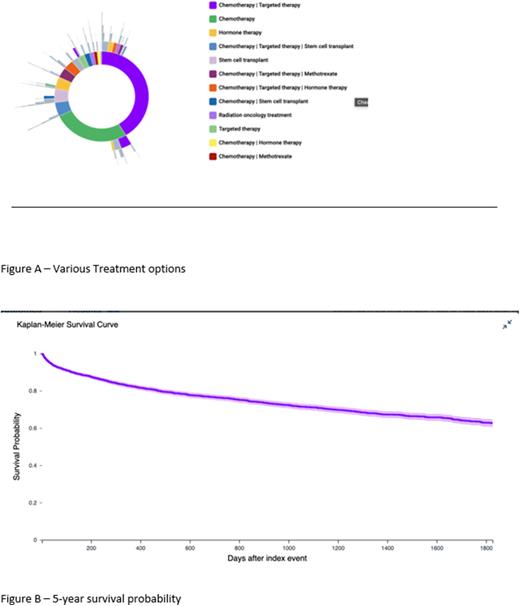
Methods: We performed a real-time search and analysis for patients (≥18 years age) diagnosed with PTLD following SOT from 1/1/2000 to 7/27/2022 by using the TriNetX (Cambridge, MA) Research Network. We examined the demographics characteristics (age, sex, race, and ethnicity), diagnoses, procedures, medications, laboratory parameters for identified patients. We calculated overall and annual incidence and prevalence of PTLD following SOT, stratified by demographic characteristics. We also calculated 1-year and 5-year survival probability following PTLD diagnosis using Kaplan-Meier curves. Finally, the treatment pathways (lines of treatment and time on treatment) were calculated and displayed using Sunburst Diagram.
Results: We identified 3,645 cases of PTLD from 49 healthcare organizations with an increasing prevalence over the past two decades. The mean (standard deviation) age at diagnosis was 51 +/- 18 years (range 18-90 years), 63% (2284) were male and 37% (1352) female. Majority of patients were White (71%) followed by Black (13%), Asian (3%), and American Indian (1%), unknown (12%). The cohort had 77% Non-Hispanic and 7% Hispanic pts. The most common organ of transplant was kidney in 59 % (2167) cases, 26% (960) were liver transplant, 12% (425) lung and 2% heart and 1% were pancreas transplant cases. Lactate dehydrogenase was high at the time of diagnosis mean (SD): 374 (+/-883) IU/l. The various treatment options included Rituximab single agent in 7.81% , Chemotherapy ( Including RCHOP, methotrexate, R-EPOCH ) in 47.2% , Stem cell transplant in 9.71%, Radiation was used in 4.91%, CAR-T cell therapy in 7 patients, second like therapy (including Tafasitimab, Polatuzumab vedotin) was used in less than 1% as shown in Figure A. The risk of 1-year mortality was 16.2% which increased to 27.68% over 5 years post diagnosis. The survival probability at 1 year and 5 year was 82% and 66%, respectively as shown in Figure B.
Conclusions: This retrospective analysis is one of the largest studies evaluating the trends in incidence, treatment pathways and survival in PTLD patients. We demonstrated increasing prevalence with highest cases seen in White male patients. Chemotherapy was the most common modality of treatment. Although newer therapies like CAR-T and targeted agents have started to be used now, the 5-year survival probability remains low. More studies are needed to identify the factors predicting outcomes and improving treatment options in this aggressive malignancy.
Disclosures
Diaz Duque:Incyte: Consultancy; Morphosys: Consultancy; ADCT: Consultancy; Astra Zeneca: Consultancy; Epizyme: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.